Advances in technology have shrunk imaging devices small enough to navigate the human body. Endoscopic optical fibres have become commonplace in medicine, giving clinicians an unprecedented insight into their patients’ health.
The state-of-the-art imaging fibres are made up of many thousands of ‘cores’, bundled together into a single fibre. Each of the cores acts like a pixel, transmitting a part of the image down the fibre to a screen outside the body. These fibres allow clinicians to visualise the smallest areas of the body with microscopic precision. However, they come at a cost. Reaching several thousands of dollars per device, they must also be sterilised between uses. This degrades the fibre limiting its lifespan, while improper sterilisation carries the risk of cross-contamination between patients.
Dr James Stone and his team have been using the Fibre Fabrication Facility to design and test low-cost optical fibres specifically for use within healthcare and medicine. Inspired by the commercially produced technology powering telecommunications, they hope to create high-quality, economically viable disposable imaging devices.
Getting started
The team began their research by working with clinicians to identify barriers to effective treatment. One of the biggest concerns raised by lung specialists is the danger posed by infection, especially in intensive care units (ICU). In an already weakened state, patients are vulnerable to infection. If they then require mechanical ventilation, their risk of infection rises, and chance of survival drops.
Ventilator-Associated Pneumonia is a catch-all term for lung infections in ventilated patients, and treatment can be harsh. Traditional diagnosis relies on growing bacterial cultures, which can take several days to identify the cause of infection. But when initial clouding on the lungs is picked up by X-rays, patients tend to deteriorate quickly. With no time to lose, clinicians often administer a suite of antibiotics and antifungals, in the hope one of them will begin to take effect.
Visualising the problem
Dr Stone’s research has been exploring the use of a bespoke, low-cost optical fibre-based delivery and imaging endoscope. Using this device, a fibre could be inserted directly into an infected lung and deliver a small amount of fluid into the field of view. This fluid contains a chemical probe that glows in contact with specific bacteria or fungi.
Through a process of elimination and testing different chemical probes to see what lights up, clinicians would be able to rapidly identify infection-causing pathogens and offer more targeted treatments.
Testing their device in ex-vivo human lungs, the team were able to identify the bacteria Staphylococcus aureus within 60 seconds of the fluid being delivered.
Creating the device
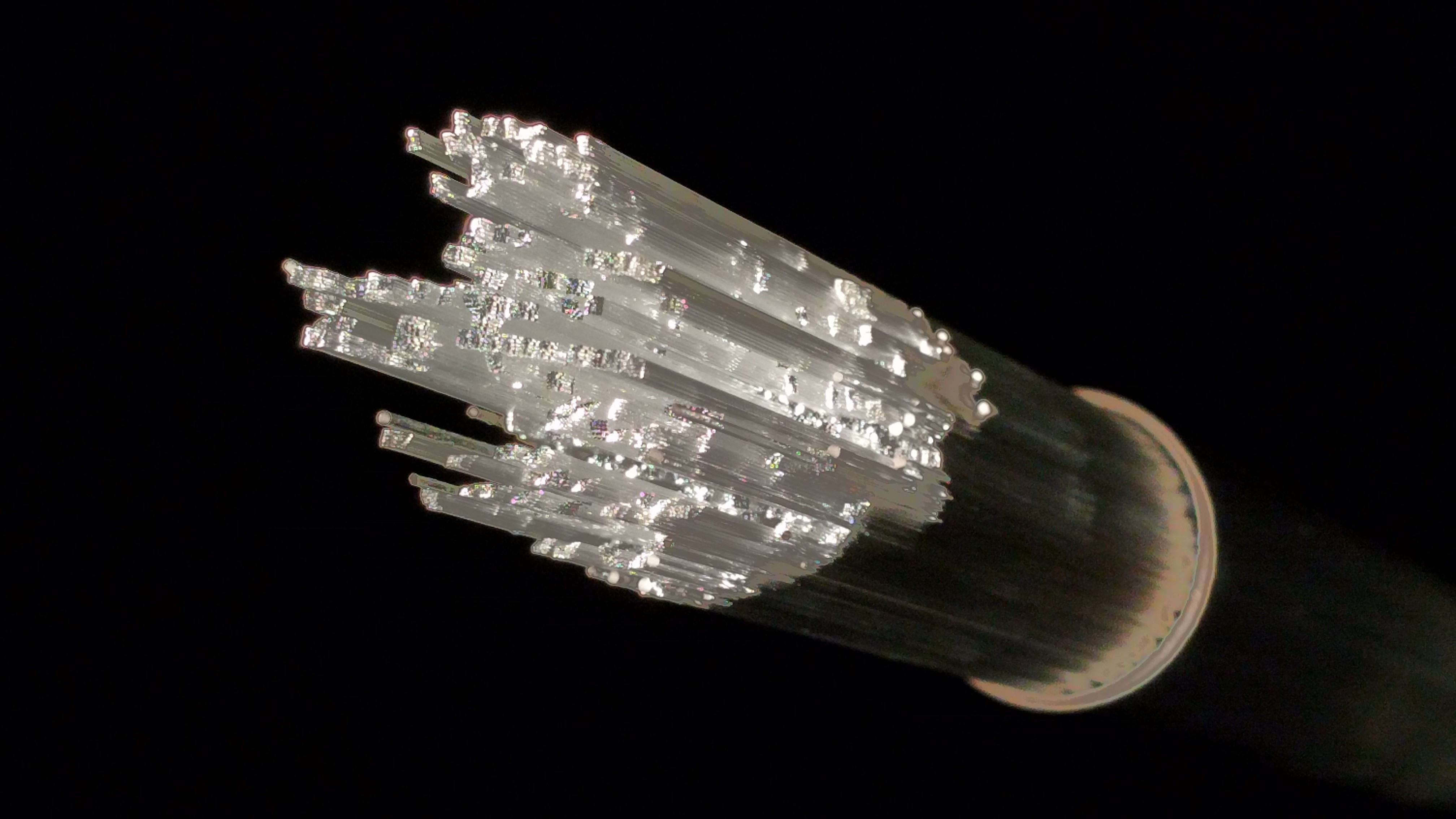
The three-in-one device comprises an imaging fibre and two fluid delivery channels, wrapped together in a polymer coating.
The imaging fibre is made using the low-cost, commercially produced preforms used by the telecommunications industry. These preforms are then drawn out into 8,100 individual cores, that are bundled together into a square formation. The cores are made with differing sizes, and stacked in a unique pattern so that no two of the same size are adjacent.
The resulting images are comparable to those produced by state-of-the-art imaging fibres.
Taking the next steps
Dr Stone’s research team are continuing to work with clinicians at the University of Edinburgh, designing fibres to tackle a range of medical problems. Each fibre is made bespoke and can only be used in devices for patients after thorough testing, starting with safety and feasibility tests.
Once designed and their concept is proven, the next step for these devices is to undergo clinical trials and hopefully commercialisation.
In the meantime, they continue to use the Fibre Fabrication Facility to optimise their fibre designs and create more for use in their research.